
Dysphagic disorder in a cohort of COVID-19 patients
Dysphagic disorder in a cohort of COVID-19 patients
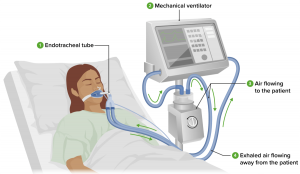
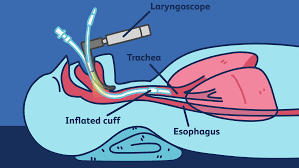
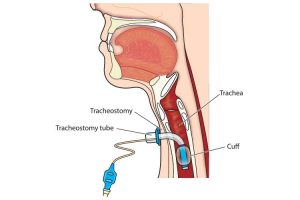
Management of COVID-19 often involves Invasive Mechanical Ventilation (MV) and in some cases a tracheostomy too. A known complication of prolonged MV and Tracheostomy is pharyngeal muscle dysfunction. Pharyngeal Muscle Dysfunction is associated with dysphagia and swallowing disorders.
Hence, it might be the case that patients who got admitted to ICU due to COVID-19-related complications may develop Dysphagia. Read the original research conducted by Ceruti and team on
The aim of this study by Ceruti and team was to understand the presence of dysphagia in critically ill COVID-19 patients. Simultaneously, describing the features of the swallowing disorders detected and the associated risk factors.
Dysphagia is difficulty swallowing. Includes taking more time and effort to move food or liquid from your mouth to your stomach. Dysphagia can be painful. In some cases, swallowing is impossible. Dysphagia can occur at any age, but it’s more common in older adults. The causes of swallowing problems vary, and treatment depends on the cause. Understand more about dysphagia here
This research studied the presence of Dyshagic Disorder among those who were affected with CIVID-19
-
Study Design
- Specifically, this was a retrospective observational study
- The authors studied dysphagia in ICU patients admitted for COVID complications in 2020
-
Dysphagia Assessment Evaluation
- They used the ‘Gugging Swallowing Screen’ test called as GUSS
- In addition, they measured Dysphagia Severity Scores in patients admitted to ICU for COVID complications
-
Evaluation Test and Timing
- GUSS Evaluation every day until complete recovery
- 0-9 Severe Dysphagia
- 10-14 Moderate Dysphagia
- 15-19 Mild Dysphagia
- 20 Absence of Dysphagia
- GUSS Evaluation every day until complete recovery
-
SLT Treatment
- One of the main aims was to reduce Oral and Pharyngeal sensitivity deficit
- In addition, therapy was provided to reduce delay of swallowing reflex start
- Furthermore, reduction of glottic closure deficit was targetted
- Also, therapy focused on improve laryngeal elevation motor skills
-
Data Recording
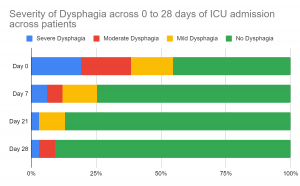
- Also, GUSS assessment performed at day 0, day 7, day 14, day 21 and day 28
- Comorbidities and other information
-
Analysis
- Descriptive and Statistical Analysis
- Describe if patients admitted in ICU post COVID developed dysphagia and required any treatment.
What were the findings from this study?
The patients admitted in ICU were on various treatments such as Mechanical Ventilator, Endotracheal Tube and Tracheostomy. These might cause Dysphagia related complications in long term. In total, 31 ICU patients were studied. Out of which, 25 were on Mechanical Ventilator, 19 were on Endotracheal Tube and 6 were on Tracheostomy.
An important finding was that at least 55% of patients admitted to ICU post-COVID 19 complications had Dysphagia. Treatment including Mechanical Ventilator led to more severe dysphagia.
Subsequently, evaluation for Severity of Dysphagia on Day 0, Day 7, Day 21, and Day 28 was recorded. Treatment for dysphagia started simultaneously. Take a look at the effects of therapy. Patients were recovering from swallowing disorders or dysphagic disorders over time with therapy (Observe the green bars over time !)
- Treatments involving Mechanical Ventilators, Endotracheal Tubes or Tracheostomy in ICU set ups may lead to Dysphagia in some people.
- In such cases, the recovery period was short despite high prevalence and severity.
- Finally, Speech Language Pathologists could play a relevant role in critically ill COVID-19 patients’ multidisciplinary management.
- “Interventions for children and adolescents with stuttering” - April 7, 2023
- What is Speech Therapy and its effect? - December 21, 2022
- Dysphagic disorder in a cohort of COVID-19 patients - December 13, 2022

Leave a Comment
(0 Comments)