
Tele-Speech Therapy for Dysarthria Management: A Case Study
Tele-Speech Therapy for Dysarthria Management: A Case Study
Dysarthria is a neurologic motor speech impairment that causes the speech musculature to be slow, weak, and/ or imprecise( Duffy 2013). Therefore, the major attribute of dysarthria is reduced speech clarity and it can be managed through different tele-speech therapy techniques. The affected individual can retain the content of the spoken language. Hence, the individual can write and comprehend spoken and written language.
Dysarthria is caused by damage to the brain or conditions that affect the nervous system. Some of these conditions e.g. include Huntington’s disease, multiple sclerosis, traumatic brain injury, etc. It can occur at any age. It is evaluated that 22% – 58% of individuals with acute stroke present with dysarthria (De Cock et al., 2021; Safaz et al., 2016; Stipancic et al., 2019) which is why tele-speech therapy for the management of dysarthria is an important topic of discussion.
A stroke is a medical emergency that significantly cuts down the flow of blood to the brain. When an adequate amount of oxygen is not supplied to the brain, degeneration of brain cells begins shortly. Numerous people who suffer a stroke exhibit similar symptoms, i.e. slurred speech, challenges with swallowing, visual deficits, and weakness or paralysis in various parts of the body. The consequences of stroke on different parts of the body generally depend on the site of the brain lesion. Speech and language therapy establishes functional communication between the speaker and their listeners, making it the cornerstone of dysarthria treatment.
The objective of Tele-Speech Therapy for the Management of Dysarthria: A Case Study was to document and discuss the tele-speech remediation of a person with dysarthria via tele-practice.
Clinical evaluation and therapy strategies of client with dysarthria.
Participant
The participant in the Tele-Speech Therapy for the Management of Dysarthria: A Case Study was a 48-year old adult male diagnosed with spastic dysarthria, post-stroke. He had a stroke on 03.12.21. Medical reports indicated cortical lesions in the brain. After medical management, he enrolled for Speech and Language intervention at SpecialPlace on 30.12.21.
Method:
1. Phase I: Speech and Language Evaluation and Oro-motor Examination
Firstly, the therapist administered a detailed case history to explore the communication profile and oro-motor skills. The participant had slurred speech with reduced rate and intelligibility. Earlier, the speech was monotonous. He reported exhaustion after conversing for more than 20 minutes evidently. Spontaneous and non-spontaneous speech contained intact language content, syntax, and semantics. There was a delay in the processing of complex sentences. At times, he mixed up numbers and alphabets in reading tasks.
The therapist conducted an oral peripheral mechanism examination to assess the structure and function of the oral cavity. Lips and tongue were slightly deviated to the right side. Lip and tongue movements were slow and restricted. Cheek muscles on the right side of the face were weak. Intra-oral breath pressure was achieved and sustained for up to 12 seconds. He reported occasional pocketing of saliva and mild drooling.
He could take fluids slowly through the straw. Intake of fluids directly from the cup was difficult. He could take semi-solid food items. Previously, his maximum phonation time was less than 5 seconds, which indicated reduced breath support for speech. His diadochokinetic rates were 4.3, 4.2, and 3.4 for /p/, /t/, and /k/, respectively.
The therapist administered Frenchay Dysarthria Assessment (FDA) to understand the severity of impairment of oro-motor structures.
2. Phase II: Speech Therapy
After the detailed evaluation for Tele-Speech Therapy for the Management of Dysarthria: A Case Study through tele-mode, the participant enrolled in speech therapy thrice a week. The therapist implemented restorative therapy strategies (Clark, 2014) to restore the function of the speech subsystems. The major areas of focus were respiration, phonation, resonance, articulation, and prosody. We conducted regular tele-speech therapy sessions via Zoom Video Communications from January 2022 to May 2022.
We trained the participant to follow slow and controlled inhalation and exhalation in order to improve respiratory control for speech. Phrase grouping and usage of maximum vowel prolongation tasks helped him improve the duration and loudness of speech. We implemented speech pattern modification to improve resonance and applied phonetic placement strategies to optimize the positioning of oral structures during speech. Pacing strategies using a metronome, application of lexical stress, and matching breaths to natural pauses in speech helped to improve prosody. The spouse regularly assisted in carrying out oromotor exercises.
These exercises improved the speed, strength, and function of the oro-motor musculature. After completing all the sessions, we shared detailed home training tips and necessary videos with the participant via email. The participant successfully followed up the home training with the support of his spouse. Apart from speech and language, the participant attended occupational therapy and physiotherapy.
Results
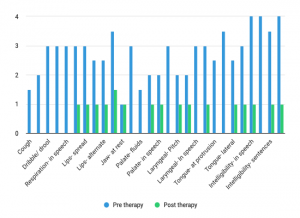
The therapist administered FDA after five months of intense speech therapy and home training. Graph- 1 represents the functioning of oro-motor structures of the participant- pre and post-therapy. The performance is portrayed on a 4 point rating scale, with ‘0’ indicating performance within the normal range and ‘4’ indicating impairment in performance. The graph illustrates that before therapy, the participant exhibited poor respiratory control and experienced affected reflexes. Oro-motor structures like lips and tongue had fair symmetry. Functions of lips, tongue, and palate were moderately to severely affected; severe effect on speech intelligibility.
After therapy, reflexes were back to normal range. The movements of the jaw, lips, tongue, and palate improved significantly. The function of these structures showed reduced impairment, with only minimal impairment remaining at the end of the fifth month of speech therapy. The strength of his cheek muscles improved, which resulted in normal intra-oral breath pressure and blowing skills. Speech intelligibility was poor, that is, the pre-therapy score showed severe impairment in speech intelligibility. Post-therapy, the speech was intelligible to familiar as well as unfamiliar communication partners. The rate of speech was back to normal.
Discussion and Conclusion
Difficulty controlling or weakness of the muscles required for speech execution results in dysarthria. Medical intervention and multi-disciplinary rehabilitation are the management options for individuals with dysarthria. The main symptom of dysarthria is unclear speech, due to the abnormal functioning of oro-motor structures. However, the condition also involves issues related to feeding. Speech therapy focuses on strengthening the oro-motor structures and improving speech clarity.
In the present study, the participant enrolled in tele-speech therapy after 15 days of stroke. This early intervention is a major factor that helped the participant to achieve drastic progress in his oro-motor and communication skills. Unquestionably, research and practical evidence have proven that during the first three months after a stroke, a patient might experience a phenomenon called spontaneous recovery. Spontaneous recovery is the process of a skill or ability that seemed lost due to the stroke returning suddenly as the brain finds new ways to perform tasks.
In the present study, the process of spontaneous recovery complemented regular tele-speech therapy and oro-motor strengthening exercises. Because of this, the participant could exhibit drastic progress in oro-motor skills and speech intelligibility. Additionally, this study revealed that tele-speech therapy for dysarthria resulted in positive progress in the speech fluency of the participant.
Read more about Dysarthria here.
- Tele-Speech Therapy for Dysarthria Management: A Case Study - September 29, 2023


Leave a Comment
(0 Comments)