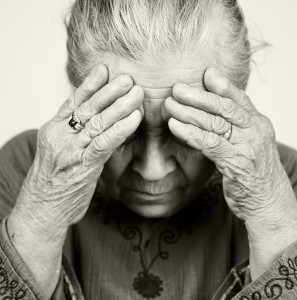
Depression in Elderly: How to Help a Parent
Depression in Elderly: How to Help a Parent
Depression can affect anyone regardless of their age, gender or any other background. While we are still yet to overcome the stigmas attached to this disease, the geriatric population in our country continues to suffer. Lack of awareness also leads to the family feeling helpless and not understanding how to help. Older people are at risk for depression, are underserved by the mental health profession, and have high rates of suicide in the country. But many seniors are resistant to treatment because they don’t want to burden their families or equate depression with weakness or even death. In such cases, it’s the family that has to take the first step and make it easier for the elderly so that they can deal with the situation more efficiently and yield better results. So how can you help your parent or a senior family member going through Depression?
1.Don’t dismiss symptoms
Depression is not normal bereavement or stress. Depression is a disease that affects mood, cognition, appetite, sleep cycle etc. If your parent is not eating for more than a few days or loses interest in activities that used to give her pleasure for more than two weeks, it could be depression.
2.Talk about how they feel
If your father can no longer drive, offering to drive him around or pay for a taxi service won’t necessarily soften the blow.
The elderly are less likely to cope with depression as well as young people because of the added years of meaning behind it.
Caregivers can help by recognizing its significance: Ask your elderly parent what they feel. It’s really important to hear them out and honor their emotions. Listening offers direct comfort and support.
3.Look for subtle signs
Instead, they show signs of distress by wringing their hands excessively, getting agitated or irritable, or having difficulty sitting still. Looking and identifying such signs will be beneficial to get help sooner.
4.Don’t impose your terminology
For the person who says, ‘No, I am not depressed,’ listen closely to what has changed in their life.
For example, if they say they can’t sleep, use that as a hook to discuss ideas about how to sleep better or longer.
It is also recommended not to say the words ‘depression,’ ‘drugs,’ or ‘therapy’ if an older adult doesn’t buy into the idea that they need help. That will make them upset or even worse might create panic.
5.Recognize that depression is an illness
Family members should be aware of the disability that depression can cause and should avoid making depressed parents or relatives feel guilty by telling them to get out more or pull themselves up by the bootstraps. Researching and reading about it will help you become more aware and prepared to deal with it.
6.Don’t take over a person’s life
7.Try to participate in medical care
- Effects of Psychotherapy on Parental Stress - November 21, 2023
- Couple’s Therapy: Navigating marital issues as a parent - June 9, 2023
- Talk Therapy for stuttering - May 31, 2023



Leave a Comment
(0 Comments)